|
Keratoconus
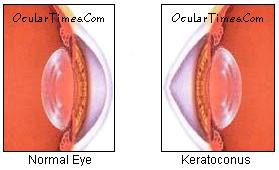
Keratoconus (ectatic corneal dystrophy) is an eye condition in which
the shape of the cornea bulges and becomes conical
(cone-shaped), resulting in thinning and eventual
scarring of the central cornea. The disorder affects
women more often than men, and occurs more frequently in
patients with Down's syndrome, Marfan's
syndrome, Addison's disease, neurofibromatosis,
allergies, and congenital amaurosis (a rare form of
blindness at birth).
Symptoms
Keratoconus
is characterized by thinning and protrusion of the
central and/or paracentral cornea, resulting in corneal
distortion, photophobia, halos around lights, decreased
vision, and monocular diplopia (double-vision).
Indicative warning signs of early keratoconus include
frequent eyeglass prescription changes associated with
progressive myopic astigmatism.
The onset of
keratoconus occurs predominantly in the late teens.
Symptoms usually appear bilaterally, but it is not
uncommon to have an asymmetric presentation. During the
first 5-7 years of onset, the condition generally worsens
with intermittent periods of remission. In many cases,
the degenerative process stops as the patient reaches his
or her 40s. The first eye affected typically suffers more
severe consequences, while the second eye may not show
any signs until years later, if at all.
On clinical
examination, patients with keratoconus may produce a low
intraocular pressure (IOP) reading. This is due to
corneal thinning and/or reduced sceral rigidity, either
of which can cause a reduction in corneal tension on
tonometer applanation.
Causes
Various
theories have speculated that biochemical abnormalities
may be responsible for the development of keratoconus.
Recent studies have shown that abnormalities in
proteoglycan metabolism have been associated with
keratoconic corneas. Abnormalities in collagen fiber
cross-linking have also been documented. There also
appears to be some association with certain systemic
diseases (see above).
Another
theory is that keratoconus represents a degenerative
condition attributed to corneal stress factors. Studies
that support this theory note that keratoconus develops
more often in persons who have a history of recurrent
ocular surface irritation secondary to long-term contact
lens wear and chronic vernal conjunctivits.
The role of
heredity in the development of keratoconus has not been
clearly established. Although genetic inheritance of the
disorder has been noted, the majority of the cases show
no definitive inheritance pattern. In some cases,
however, genealogical analysis suggests a sex-linked
autosomal dominant mode of inheritance, particularly
because of the predominance of familial females with
keratoconus
Diagnosis
Early
keratoconus usually manifests as a small island of
irregular astigmatism in the inferior paracentral cornea.
As the cornea bulges outward, the amount of astigmatism
increases due to the progressive distortion of the
corneal surface. These changes can easily be seen as
irregular mires on keratometry readings and on corneal
topography, a test used to map the topographical
surface area of the cornea.
 Munson's
sign - On physical examination, Munson's Sign
is readily observable without the requirement of
sophisticated testing equipment. As the patient gazes inferiorally, the apex of the cone angulates the lower
lid outward, forming a 'V-shaped' protrusion. Milder
signs of Munson's may be more easily seen when the head
is tilted slightly back and upper lids are lifted while
the patient gazes downward. Munson's
sign - On physical examination, Munson's Sign
is readily observable without the requirement of
sophisticated testing equipment. As the patient gazes inferiorally, the apex of the cone angulates the lower
lid outward, forming a 'V-shaped' protrusion. Milder
signs of Munson's may be more easily seen when the head
is tilted slightly back and upper lids are lifted while
the patient gazes downward.

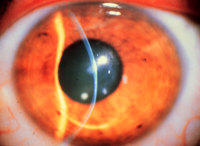
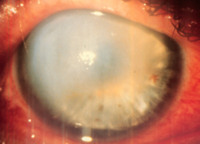
Corneal Hydrops -
usually seen in more advanced cases of keratoconus;
occurs when Descemet's membrane (a layer within the
corneal strata) is stretched beyond its breaking point
and ruptures. The influx of fluid from the aqueous
results in significant corneal edema and opacification (a
whitish-opaque spot appears on the cornea). Hydrops can
cause severe pain and significantly reduced vision.
Descemet's membrane regeneration is slow. As the membrane
layer regenerates, the edema and opacification gradually
resolve, but a scar formation will often remain on the
cornea. In some cases, hydrops can occur suddenly while
rubbing the eye.
KERATOCONUS
Keratoconus has no known cure, and
many people do not even know they have it because it begins as nearsightedness
and astigmatism. It is a progressive disorder that may progress rapidly or
sometimes take years to develop. It can severely affect the way we see the
world, including simple tasks such as driving, watching TV, or just reading a
book. Some keratoconus patients have described their vision as being “blind
with light.”
Keratoconus is a non-inflammatory,
self-limiting ectasia of the axial portion of the cornea. It is characterized by
progressive thinning and steepening of the central cornea. As the cornea
steepens and thins, the patient experiences a decrease in vision which can be
mild or severe depending on the amount of corneal tissue affected.
Onset of keratoconus occurs during
the teenage years--mean age of onset is age 16 years--but onset has been
reported to occur at ages as young as 6 years. Keratoconus rarely develops after
age 30 years. Keratoconus shows no gender predilection and is bilateral in over
90% of cases. In general, the disease develops asymmetrically: diagnosis
of the disease in the second eye lags about five years after diagnosis in the
first. The disease process is active for about five to 10 years, then it may be
stable for many years. During the active stage, change may be rapid.
Typically, vision loss can be
corrected early by spectacles; later, irregular astigmatism requires optical
correction with rigid contact lenses. Contact lenses provide a uniform
refracting surface and therefore improve vision. Contact lenses can improve
vision, but they can also scar the cornea. Patients should be informed upon
diagnosis that they will likely require contact lenses eventually. Although most
patients can continue to read and drive, some feel quality of life is adversely
affected. Patients need to know that eye examinations will be required annually
or more frequently to monitor progression. About 20% of patients will eventually
need a corneal transplant.
Etiology
The proposed etiology of
keratoconus includes biochemical and physical corneal tissue changes, but no one
theory fully explains the clinical findings and associated ocular and non-ocular
disorders. It is possible that keratoconus is an end result or final common
pathway of many different clinical conditions. It has been found in association
with hereditary predisposition, atopic disease, certain systemic disorders, and
long-term rigid contact lens wear.
Diagnosis
Identifying moderate or advanced
keratoconus is fairly easy. However, diagnosing keratoconus in its early stages
is more difficult, requiring a thorough case history, a search for visual and
refractive clues and the use of instrumentation. Often, keratoconus patients
have had several spectacle prescriptions in a short period, and none has
provided satisfactory vision correction. Refractions are often variable and
inconsistent. Keratoconus patients often report monocular diplopia or polyopia
and complain of distortion rather than blur at both distance and near vision.
Some report halos around lights and photophobia.
Many objective signs are present
in keratoconus. Retinoscopy shows a scissoring reflex. Direct ophthalmoscopy may
show a shadow (Fig. 1). If the pupil is dilated and a +6.00 D
lens is in the ophthalmoscopic system, the cone may appear as an oil or honey
droplet when the red reflex is observed.
Fig 1.

The keratometer also aids
diagnosis. The initial keratometric sign of keratoconus is absence of
parallelism and inclination of the mires. These can easily be missed in mild or
early cases. As the cornea advances, the mires appear smaller. To extend the
range of the keratometer, an ancillary lens is placed on the front of the
keratometer . If a +1.25 D lens is used, this extends the range to 60 D. To
record a reading, 8 D is added to the drum reading (for example, if the drum
reads 45 D, adding 8 D yields an actual reading of 53 D). A +2.25 D lens extends
the range to 68 D by adding 16 D to the reading.
The photokeratoscope or
topographer placido disc can provide an overview of the cornea and can show the
relative steepness of any corneal area. Figure 2 depicts the
keratoconic cornea. The even separation of the rings in the spherical and the
astigmatic cornea and the uneven spacing of the rings--especially inferiorly--in
the keratoconic cornea should be noted. The central rings may show a tear-drop
configuration termed "keratokyphosis".
Reduced visual acuity in one eye,
due to the disease's asymmetry, may be a clue with the early keratoconus
patient. This sign is often associated with oblique astigmatism. In early
keratoconus, the patient may become less myopic six months later as the
astigmatism increases.
 |
 |
| Normal
keratoscopy |
Early keratoconus |
 |
| Moderate
keratoconus |
Keratoconus can result in
extremely complex and variable topographical maps, most typically showing areas
of inferior steepening. The cone can assume various shapes and sizes, and the
apex can be at various locations in relation to the central cornea.
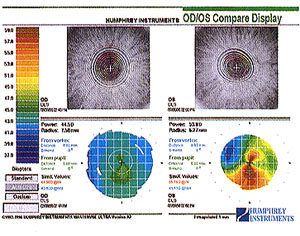
Placido's computerized video
topography showing unilateral early keratoconus
SLIT-LAMP DETECTION
The biomicroscope is the only tool
which allows a clinician to observe many classical signs of keratoconus:
Fleischer's ring, stress lines of Vogt, corneal thinning and scarring, various
types of staining with and without lens wear, increased visibility of corneal
nerves, and corneal hydrops.
Fleischer's Ring
The Fleischer ring is a
yellow-brown to olive-green ring of pigment which may or may not completely
surround the base of the cone (Fig. 3). Formed when hemosiderin
(iron) pigment is deposited deep in the epithelium , Fleischer's ring often
becomes thinner and more discrete with progression. A careful inspection of the
keratoconic cornea will reveal a line in approximately 50% of all cases.
Locating this ring initially may be made easier by using a cobalt filter and
carefully focusing on the superior half of the cornea's epithelium. Once
located, the ring should be viewed in white light to assess its extent.
Fig 3.

Lines of Vogt
Lines of Vogt are small and
brushlike lines, generally vertical but they can be oblique. These lines can be
found in the deep layers of the keratoconic stroma (Fig. 4) and
form along the meridian of greatest curvature; the lines
disappear when gentle pressure is exerted on the globe through the lid. Lines of
Vogt are more easily viewed when they reappear after this pressure is removed.
Rigid lens wear sometimes accentuates the lines. In advanced cases of
keratoconus, posterior corneal folds may also be present.
Fig 4.
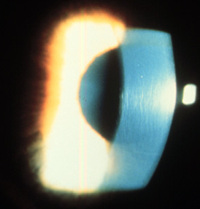
Corneal Thinning
Significant thinning (up to 1/5th
cornea thickness) in the advanced stages of the disease (Fig. 5),
and a diagnostic criterion based on comparison of central and peripheral corneal
thickness has been proposed. Additionally, as the disease progresses, the cone
is often displaced inferiorly. The steepest part of the cornea (apex) is
generally the thinnest. Apical thinning described is believed to represent an
actual reduction in the number of stromal lamellae rather than an overall
thinning process.
Fig 5.
Corneal Scarring
Sub-epithelial corneal scarring,
not generally seen early, may occur as keratoconus progresses because of
ruptures in Bowman's membrane which is then filled with connective tissue (Fig.
6). Deep opacity of the cornea are not uncommon in keratoconus. It has
also been reported that flat-fitting contact lenses may produce or accelerate
corneal scarring. A raised "callous" is possible but is easily treated
by simple debridement or laser ablation. In addition, apical scarring with an
overlying epithelial defect and surrounding edema can be confused for ulcerative
keratitis in this disease process.
Fig 6.

Swirl Staining
Swirl staining may occur in
patients who have never worn contact lenses because basal epithelial cells drop
out and the epithelium slides from the periphery as the cornea regenerates.
Thus, a hurricane, vortex, or swirl stain may occur (Fig. 7).
Swirl staining may be due to rubbing of the eye or can also result from flat-
fitting contact lenses. When this is the case, the lens is generally too flat. A
steeper lens often diminishes staining.
Fig 7.

Hydrops
Corneal hydrops occurs, generally
in advanced cases, when Descemet's membrane ruptures, aqueous flows into the
cornea and reseals (Fig. 8). Keratoconus patients who are
having an acute episode of corneal hydrops report a sudden loss of vision and a
visible white spot on the cornea. Corneal hydrops causes edema and opacification.
As Descemet's regenerates, edema and opacification diminish. Occasionally,
hydrops can benefit keratoconus patients who have extremely steep corneas. If
the cornea scars, a flatter cornea often results, making it easier to fit with a
contact lens. An increased incidence of hydrops has also been reported in
keratoconus patients with Down's syndrome. Excessive rubbing should be
discouraged in this population. Anecdotally, hydrops seemed to be more prevalent
when scleral lenses were employed as a treatment option.
Fig 8.
Munson's Sign
Munson's sign is readily
observable without using the slit lamp (Fig.9). This sign
occurs in advanced keratoconus when the cornea protrudes enough to angulate the
lower lid during inferior gaze.
Fig 9.

Ruzutti's Light Reflex
A light reflex projected from the
temporal side will be displaced beyond the nasal limbal sulcus when high
astigmatism and steep curvatures are present. Although not a pathognomonic sign,
Ruzutti's reflex may aid in a diagnosis especially when a biomicroscope or other
tools to aid in diagnosis are not available.
Reduced Intraocular Pressure
A low intraocular pressure is
generally found. This is a result of a thinner cornea and/ or reduced scleral
rigidity. Due to possible artifact and since the reliability of readings are in
question caution must be taken in carefully observing nerve fiber layers and the
overall health of the optic nerve.
Classification
Keratoconus can be classified by
cone shape, central keratometric reading, or progression. The simplest
classification systems are based on keratometric reading or shape:
Based on severity of curvature
Based on shape of cone
Surgical Treatments
Various types of surgery are
available for the patient with keratoconus. Penetrating keratoplasty
is the most common. In this procedure, the keratoconic cornea is prepared by
removing the central area of the cornea, and a full-thickness corneal button is
sutured in its place Usually, trephines between 8.0-8.5 mm are used. Fleischer's
ring can be used as the limit of the conical cornea. Generally, the second eye
is not grafted until the first eye is successfully rehabilitated. Running
sutures, using Merseline, anchored by cardinal sutures provide excellent results
(clear, compact grafts). Older patients with a slower healing response and
altered tear film generally do better with nylon and interrupted sutures for
selective removal. Contact lenses are often required after this procedure for
best visual correction.
An alternative is lamellar
keratoplasty, a partial corneal transplant. The cornea is removed to
the depth of posterior stroma, and the donor button is sutured in place. This
technique is technically difficult, and visual acuity is inferior to that
obtained after penetrating keratoplasty. As a result, use of lamellar
keratoplasty is largely confined to the treatment of large cones or keratoglobus
when tectonic support is needed. This technique requires less recovery time, and
poses less chance for corneal graft rejection or failure. Its disadvantages
include vascularization and haziness of the graft.
· Corneal Transplant
When good
vision can no longer be attained with contact lenses or
intolerance to the contact lens develops, corneal
transplantation (penetrating keratoplasty) is recommended.
In this procedure, the central area of the keratoconic
cornea is removed, and a full-thickness donor corneal
button is sutured in its place. Contact lenses are often
required after this procedure for best visual correction.
An
alternative is lamellar keratoplasty,
a partial corneal transplant. The cornea is removed to
the depth of posterior stroma, and the donor button is
sutured in place. This technique is technically
difficult, and visual acuity is inferior to that obtained
after penetrating keratoplasty. As a result, use of
lamellar keratoplasty is largely confined to the
treatment of large cones or keratoglobus when tectonic
support is needed. This technique requires less recovery
time, and poses less chance for corneal graft rejection
or failure. Its disadvantages include vascularization and
haziness of the graft.
For patients
with no scarring near the center of the cornea and 20/40
vision or better with contact lenses, another option is
surgically grafting a layer of epithelial cells to
flatten the cone-shaped cornea. This process is called epikeratophakia.
It has comparable results to corneal transplantation and,
if unsuccessful, it can be followed with corneal
transplantation.
· Corneal Implants
Intrastromal
corneal ring segments (INTACS) are currently being studied as an
option for the treatment of decreased vision in
keratoconus patients. INTACS are implanted into the
periphery of the cornea, producing a flattening effect to
the central cornea that results in a smoother contour of
the corneal surface. The advantage to INTACS is that the
ring segments can be removed should any adverse effects
arise following the implant procedure, or if improved
vision is not successfully obtained.
· Laser
Excimer laser
procedures may have some potential merit, having been
used recently with some success in removal of nodular
"callous" plaques of the central cornea. New
developments in excimer corneal modeling may allow
lamellar onlay or penetrating grafts to be lathed,
thereby eliminating refractive ametropia following
various surgical procedures.
THE GENETICS OF KERATOCONUS
In the keratoconic cornea, a possible genetic
predisposition to increased sensitivity to apoptotic
mediators by keratocytes has also been hypothesized.
Click
here for Keratoconus
Statistics
Sources
* Yuksel Totan, Osman Cekic, Erdinc
Aydin. Incidence of keratoconus in subjects
with vernal keratoconjunctivitis: A videokeratographic
study. Ophthalmology 2001; 108:824-827.
* Wilson SE, Lin DTC, Klyce SD. Corneal
topography of keratoconus. Cornea 1991; 10:
2-8.
|